Abstract
Background: Hydroxyurea (HU) is the primary medication used to prevent the significant medical and neurologic morbidities of pediatric sickle cell disease (SCD; HbSS or HbSB0 thalassemia). Despite the benefits of HU, it remains under‐utilized likely due to lack of clinician knowledge/training and negative caregiver perceptions. Thus, we developed the Engage-HU randomized controlled trial (NCT03442114) as a novel approach to address HU utilization barriers. Engage-HU is designed to assess how clinicians can engage caregivers in a shared discussion that considers their values, preferences, and scientific evidence about HU.
The COVID-19 pandemic has resulted in significant changes to healthcare delivery for children with SCD, as they are at increased risk of severe illness from COVID-19 infection. Given their risk status, it was recommended that patients with SCD complete telehealth visits when possible. Some families also chose to delay care because they feared their child would get infected at hospitals/healthcare clinics that care for COVID-19 positive patients. Since the lives of all families enrolled in the Engage-HU trial have been affected to some extent, we incorporated measures to capture the impact of the COVID-19 pandemic and the usability of telemedicine implementation and services.
Methods: Engage-HU is a randomized control trial comparing two dissemination methods for clinicians to facilitate shared decision-making with caregivers of young children with SCD. Study outcomes include caregiver confidence in decision-making and perceptions of experiencing shared decision-making as well as HU uptake and child health outcomes. Eligible children are 0 to 5 years, candidates for HU, and their caregiver has not decided about HU in the past 3 months. The trial is being conducted at 9 sites in the United States and uses a unidirectional crossover design. The primary endpoints are caregiver decisional uncertainty and caregiver perception of shared decision-making measured using validated tools. Data will be analyzed using the intent-to-treat principle, and all participants will remain in the arm to which they were randomized. A multiple group comparison analysis will be performed to assess significant response variable differences by group randomization.
The Engage-HU study aims to recruit 174 caregivers who are considering initiating HU. The trial is being conducted at 9 sites in the United States. Data collection is ongoing, and 160 caregiver-participants have been enrolled to date. Since May 2020, caregiver-participants have completed the COVID-19 Exposure and Family Impact Scales (CEFIS), which contain 2 subscales (exposure to potentially traumatic aspects of the pandemic, impact on families), and the COVID-19 telemedicine use survey during a study visit.
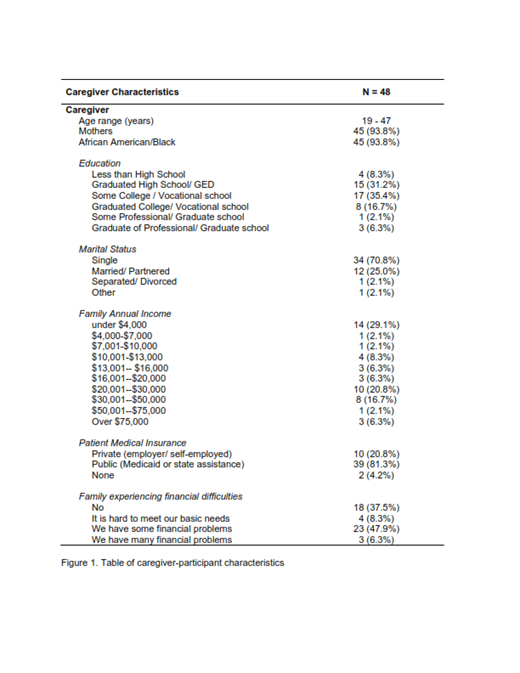
Results: Currently, 8 of the 9 sites have collected data from 48 caregivers (93.8% mothers), most of whom (93.8%) identify as African American/Black (see Figure 1). Correlations indicated that older caregivers experienced greater exposure (Mean = 7.0, SD = 4.1, range = 1-19) to potentially traumatic aspects of the pandemic (r = .31, p = .04). Distress related to COVID-19 varied widely across the sample, for both caregivers (Mean = 5.9, SD = 2.9, range = 1-10) and children (Mean = 4.1, SD = 3.4, range = 1-10). Scores on the telemedicine usability survey were generally high, indicating that caregivers are happy with the quality of care delivered via telehealth. However, caregivers (r = .30, p = .09) and children (r = .32, p = .07) experiencing more pandemic-related distress reported less satisfaction with telehealth.
Conclusion: Although Engage-HU has resumed research operations, recruitment has not reached pre-pandemic targets, as fewer eligible patients are scheduled for routine care visits at SCD clinics. Our preliminary analyses suggest a significant continued impact of the pandemic on families and general satisfaction with the quality of healthcare delivered via telemedicine. These findings indicate that targeted screenings to identify and intervene for those who demonstrate more COVID-19 pandemic-related distress are needed.
Quinn: Forma Therapeutics: Consultancy; Aruvant: Research Funding; Novo Nordisk: Consultancy; Emmaus Medical: Research Funding. Yates: Agios Pharmaceuticals: Current Employment. Badawy: Sanofi Genzyme: Consultancy; Vertex Pharmaceuticals Inc: Consultancy; Bluebird Bio Inc: Consultancy. Thompson: bluebird bio, Inc.: Consultancy, Research Funding; Baxalta: Research Funding; Biomarin: Research Funding; Celgene/BMS: Consultancy, Research Funding; CRISPR Therapeutics: Research Funding; Vertex: Research Funding; Editas: Research Funding; Graphite Bio: Research Funding; Novartis: Research Funding; Agios: Consultancy; Beam: Consultancy; Global Blood Therapeutics: Current equity holder in publicly-traded company. Smith-Whitley: Global Blood Therapeutics: Current Employment. King: National Cancer Institute: Research Funding; National Heart, Lung, and Blood Institute: Research Funding; Health Resources and Services Administration: Research Funding; Global Blood Therapeutics: Research Funding. Meier: CVS Caremark: Consultancy; Forma Therapeutic: Membership on an entity's Board of Directors or advisory committees; NovoNordisk: Membership on an entity's Board of Directors or advisory committees; Novartis,: Other: Data Safety Monitoring Board membership; NHLBI: Other: Data Safety Monitoring Board membership; Global Blood Therapeutics: Other: Steering Committee membership, grant funding; CDC,: Other: grant funding; Indiana Department of Health: Other: grant funding . Tubman: Global Blood Therapeutics: Consultancy, Research Funding; Novartis Pharmaceuticals: Honoraria, Research Funding; Forma Pharmaceuticals: Consultancy; Perkin Elmer: Honoraria. Crosby: Forma Therapeutics: Honoraria; PCORI: Research Funding; HRSA: Research Funding; Global Blood Therapeutics Panel: Honoraria; Children's Hospital of Philadelphia: Honoraria; Professional Resource Exchange: Patents & Royalties: $30-$60 every other year; SCDAA: Honoraria; NHLBI: Other: Payment for review of LRP Proposals, Research Funding.
Hydroxyurea has been FDA approved for the treatment of sickle cell disease for patients ages 2 years and above but NHLBI and ASH Guidelines recommend it be offered to children as young as age 9 months.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal